Posts for tag: tooth decay

If you've ever had a run-in with cavities, you know the drill (no pun intended): After getting a local anesthetic for pain, the dentist removes any decayed dental tissue, as well as some healthy tissue, and then fills the cavity to restore the tooth. It's an effective treatment protocol we've been using for well over a century.
It does, however, have its drawbacks. For one, although necessary, removing healthy dental tissue can weaken the overall tooth structure. The dental drill used during the procedure is also unpleasant to many people: Although it doesn't cause any pain thanks to the anesthetic, the sounds and pressure sensations associated with it can be unsettling.
But advances in dental tools, technology and techniques are addressing these drawbacks in traditional tooth decay treatment. In other words, treating a tooth with cavities today is taking on a lighter touch. Here are 3 reasons why.
Earlier detection. The key to effective treatment is to find tooth decay in its earliest stages. By doing so, we can minimize the damage and reduce the extent of treatment needed. To do this, we're beginning to use advanced diagnostic tools including digital x-rays, intraoral cameras and laser fluorescence to spot decay, often before it's visible to the naked eye.
Re-mineralizing enamel. One of the advantages of early detection is to catch tooth enamel just as it's undergoing loss of its mineral content (demineralization) due to contact with acid. At this stage, a tooth is on the verge of developing a cavity. But we can use minimally invasive measures like topically applied fluoride and CPP-ACP (a milk-based product) that stimulates enamel re-mineralization to prevent cavity formation.
Less invasive treatment. If we do encounter cavities, we no longer need to turn automatically to the dental drill. Air abrasion, the use of fine substance particles under high pressure, can precisely remove decayed material with less loss of healthy tissue than a dental drill. We're also using newer filling materials like composite resins that don't require enlarging cavities as much to accommodate them.
These and other techniques—including laser technology—are providing superior treatment of tooth decay with less invasiveness. They can also make for a more pleasant experience when next you're in the dentist's chair.
If you would like more information on effectively treating dental disease, please contact us or schedule an appointment for a consultation. You can also learn more about this topic by reading the Dear Doctor magazine article “Minimally Invasive Dentistry.”

For over a century dentists treated tooth decay by removing both diseased portions of the tooth and healthy structure deemed at risk for future decay. In the 1970s, though, a new approach emerged, known as Minimally Invasive Dentistry (MID). This practice protocol attempts to preserve as much of the healthy structure as possible.
Before MID, dentists followed a decay treatment protocol developed in the 19th Century. A part of this became known as extension for prevention calling for dentists to remove healthy structure considered vulnerable to decay. Besides reducing the tooth's volume, this practice also resulted in, by today's standards, larger than necessary fillings.
It was thought that removing this additional material would make it easier to clean bacterial plaque, the source of decay, but later, research showed the practice couldn't guarantee the teeth wouldn't be reinfected.
Since then we've learned a lot more about teeth and have developed new ways to detect decay at earlier stages. X-ray imaging, for example, has transitioned largely from film to digital technology, providing more detailed images at greater magnification. This, along with laser fluorescence and infrared cameras, has made it easier to detect the first tiny stages of decay.
We can also limit tooth decay damage by boosting enamel strength with fluoride applications and sealants or reducing decay-causing bacteria with anti-bacterial rinses. We've also seen advancement in techniques like air abrasion that remove decayed tooth material while leaving more healthy structure intact better than using a traditional dental drill.
Restoring teeth after treatment has also improved. While dental metal amalgam is still used for some fillings, the main choice is now composite resin. These new tooth-colored dental materials require less tooth preparation (and thus less material loss) and bond well to the remaining structure, resulting in a stronger tooth.
Following a MID protocol leads to less intervention and less time in the dentist's chair. It also means preserving more of a natural tooth, an important aim in promoting long-lasting dental health.
If you would like more information on minimally invasive dentistry, please contact us or schedule an appointment for a consultation.
Tooth decay is one of two dental diseases most responsible for tooth loss (gum disease being the other). In the absence of treatment, what starts as a hole or cavity in a tooth's outer layers can steadily advance toward its interior.
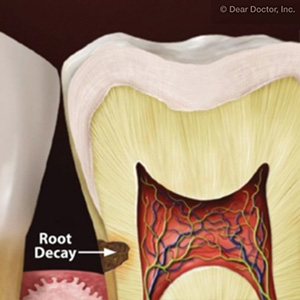
Most people associate cavities with the crown, the part of a tooth you can see. But cavities can also occur in a tooth's roots, especially with older adults. Root cavities pose two distinct difficulties: They can lead to more rapid decay spread than crown cavities within a tooth; and they're harder to detect.
Tooth roots are ordinarily covered by the gums, which protects them from bacterial plaque, the main cause for decay. But roots can become exposed due to receding gums, a common problem with seniors who are more susceptible to gum disease.
Unlike the enamel-covered crowns, tooth roots depend on gum coverage for protection against bacteria and the acid they produce. Without this coverage, the only thing standing between tooth decay and the roots is a thin material called cementum.
If decay does enter a tooth's interior, saving it often requires a root canal treatment to remove decayed tissue in the inner pulp and root canals, and then replacing it with a filling. But if we're able to discover a root cavity in its early stages, we may be able to fill it like a crown cavity.
The best strategy, though, is to prevent root cavities from forming. This starts with a dedicated daily regimen of brushing and flossing to remove dental plaque. If you're at high risk for root cavities, we may also recommend antibacterial mouthrinses and other aids.
Regular dental visits are also a must: a minimum of twice-a-year dental cleanings to remove stubborn plaque and calculus (hardened plaque) deposits. For added protection against root cavities, we can also apply fluoride varnish to strengthen teeth. And regular visits are the best way to detect any cavity in its early stages when treatment is less invasive.
A heightened risk of dental problems like root cavities are a part of the aging process. But partnering together, we can lower that risk and increase the longevity of your teeth.
If you would like more information on root cavities, please contact us or schedule an appointment for a consultation. You can also learn more about this topic by reading the Dear Doctor magazine article “Root Cavities.”
Although preventable, the occurrences of tooth decay are all too common. Yet decay doesn’t appear out of the blue: certain mouth conditions set the disease in motion.
Here are a few signs of such conditions to watch for — they could be telling you you’re at higher risk for tooth decay.
Visible plaque. Plaque is a thin film of bacteria and food accumulating on tooth surfaces and a prime haven for causing periodontal disease. If you actually see it — a crusty, yellowish film — that means there’s a large, unhealthy amount of it. It’s essential to remove it daily through diligent brushing and flossing and more thorough office cleanings at least twice a year.
Poor saliva flow. One of this bodily fluid’s functions is to neutralize mouth acid, usually thirty minutes to an hour after we eat. If saliva flow is inadequate, though, acid levels may remain high and endanger the enamel. “Dry mouth” can occur from a number of causes, including some medications and chemotherapy treatments. It’s important to alleviate the cause if possible by changing medications or stimulating saliva flow through other means.
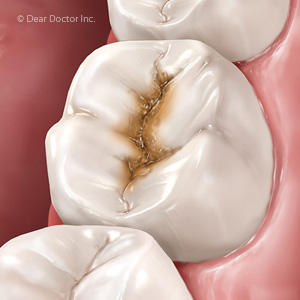
Tooth shape and appliances. Largely determined by heredity, your teeth contain unique, tiny grooves known as pits and fissures that could harbor plaque. Certain appliances like retainers, braces or night guards can inhibit saliva flow and cause your teeth to retain more plaque. It’s important then to adjust your hygiene efforts to offset these anatomical or treatment factors.
Acid-producing conditions. Diseases like gastro-esophageal reflux disease (GERD) or eating disorders can introduce stomach acid into the mouth that is highly erosive to tooth enamel. It’s imperative for you or a family member to control these conditions through medication, dietary changes, or — in the case of eating disorders — behavioral therapy.
Eating habits. Sugar and other carbohydrates are a ready food source for bacteria. Likewise, acidic foods and beverages (like coffee, tea, and sports or energy drinks) can cause high acid levels for too long. Cut back on eating and drinking these foods and beverages, especially as snacks, to reduce acid levels that could lead to decay.
If you would like more information on strategies to prevent tooth decay, please contact us or schedule an appointment for a consultation. You can also learn more about this topic by reading the Dear Doctor magazine article “Tooth Decay: How to Assess Your Risk.”

True or false: there’s no cause for concern about tooth decay until your child’s permanent teeth erupt.
False—decayed primary teeth can lead to potentially serious consequences later in life.
Although “baby” teeth last only a few years, they’re essential to future dental health because they act as placeholders and guides for the incoming permanent teeth. If they’re lost prematurely due to decay, other teeth may drift into the empty space intended for the emerging permanent tooth. Because of this, inadequate space will crowd the out of proper alignment.
And because they have thinner enamel than permanent teeth, primary teeth are more susceptible to decay. Once decay sets in, it can spread rapidly in a matter of months.
Fortunately, we may be able to prevent this from happening to your child’s primary teeth with a few simple guidelines. It all begins with understanding the underlying causes of tooth decay.
Tooth decay begins with bacteria: As a result of their digestion, these microorganisms secrete acid that at high levels can erode tooth enamel. The higher the population of bacteria in the mouth, the higher the acidity and potential threat to the teeth.
The first objective then in preventing decay is to remove dental plaque, the thin film of bacteria and food particles on tooth surfaces, through daily brushing and flossing. And because bacteria feed on sugar as a primary food source, you should reduce your child’s sugar consumption by restricting it to only meal times and not sending your child to bed with a bottle filled with a sugary liquid (including formula or breast milk).
To help boost your child’s protection, we can also apply sealants and fluoride to teeth to help protect and strengthen their enamel from acid attack. Because we’ll also monitor for signs of decay, it’s important to begin regular dental visits beginning around age one. If we do detect decay, we can then treat it and make every effort to preserve your child’s primary teeth until they’ve completed their normal life cycle.
By taking these steps, we can help make sure your child’s early teeth go the distance. Their current and future dental health will certainly benefit.
If you would like more information on prevention and treatment of tooth decay, please contact us or schedule an appointment for a consultation. You can also learn more about this topic by reading the Dear Doctor magazine article “Do Babies Get Tooth Decay?”
